Norfolk Drug and Alcohol Partnership
In June 2022 the Government launched its latest drug strategy From Harm to Hope: a 10 year drugs plan to cut crime and save lives. This strategy was developed on the back of a two-part review undertaken by Dame Carol Black.
As part of this strategy every area in England has been tasked with setting up a partnership that will be responsible for delivering the outcomes of the strategy in a way that is best suited to its population.
In Norfolk this is called NDAP, the Norfolk Drug and Alcohol Partnership. It is made up of a wide range of organisations and services which have come together to improve outcomes for people with substance misuse problems.
The national strategy has three priority areas:
- Break drug supply chains
- Deliver a world-class treatment and recovery system
- Reduce the demand for recreational drugs
In Norfolk, we also recognise the impact that alcohol misuse can have on local people, which is why our local partnership covers both drugs and alcohol.
Substance misuse has profound and wide-ranging impacts on people’s wellbeing, their quality and length of life, on the social dynamics in families and communities, on the health and justice systems, and on the economy. Recreational substance use, even at a level associated with low risk to one’s own health, can have strong negative impacts on society through crime, violence and exploitation.
Based on applying rates from national surveys in 2021/22 to Norfolk: Around 44,000 individuals aged 16-59 took a drug. Around 13,000 people took a Class A drug such as heroin, methadone, cocaine or ecstasy. Cannabis is by far the most used drug overall. Nationally, data shows that there was a decrease in Class A drug use in the most recent years. Drug misuse typically affects younger people more than older people.
Around 190,000 adults in Norfolk drank more than the recommended maximum number of weekly units. Nationally, there is a continued trend towards drinking less in young people.
Health outcomes are worse in more deprived areas of Norfolk, and risk factors which increase people’s vulnerabilities are more prevalent in the most deprived areas, which are predominantly urban. Many people with substance misuse problems have mental ill health and vice versa, and co-existing misuse of multiple substances is common. Groups particularly vulnerable to the negative impacts of substance misuse include certain ethnic minority groups, homeless people, sex workers and people that have been in contact with the Criminal Justice System.
Children and young people are vulnerable to negative impacts of substance misuse. Substance use is associated with riskier behaviours, and early onset of substance use may lead to problematic use later in life. Risk factors such as parental substance misuse, school exclusion, childhood trauma and poor mental health may also increase the chances of substance misuse in young people. They may also be at risk of exploitation through County Lines activity. Overall, issues relating to substance misuse tend to be lower for young people in Norfolk compared to the national average.
Specialised treatment can improve health and social outcomes of those with drug and alcohol issues. In Norfolk, around 4,400 adults are in structured substance misuse treatment. It is estimated that this represents around half of all adults with a treatment need for opiate and/or crack cocaine dependency, and around one in five of all adults with an alcohol treatment need.
In the last five years, the proportion of Norfolk residents who are in treatment for opiate misuse has shown a decreasing trend, whereas the number of those seeking help for non-opiate and alcohol misuse has increased. Compared to the England average, relatively more treatment users mention problematic alcohol use.
The early phases of the Covid-19 pandemic appear to have resulted in more high-risk drinking. Fewer social interactions probably resulted in less substance use in young people during lockdowns. Early survey data indicates a return to pre-pandemic behaviours, but the long-term effects can’t yet be understood.
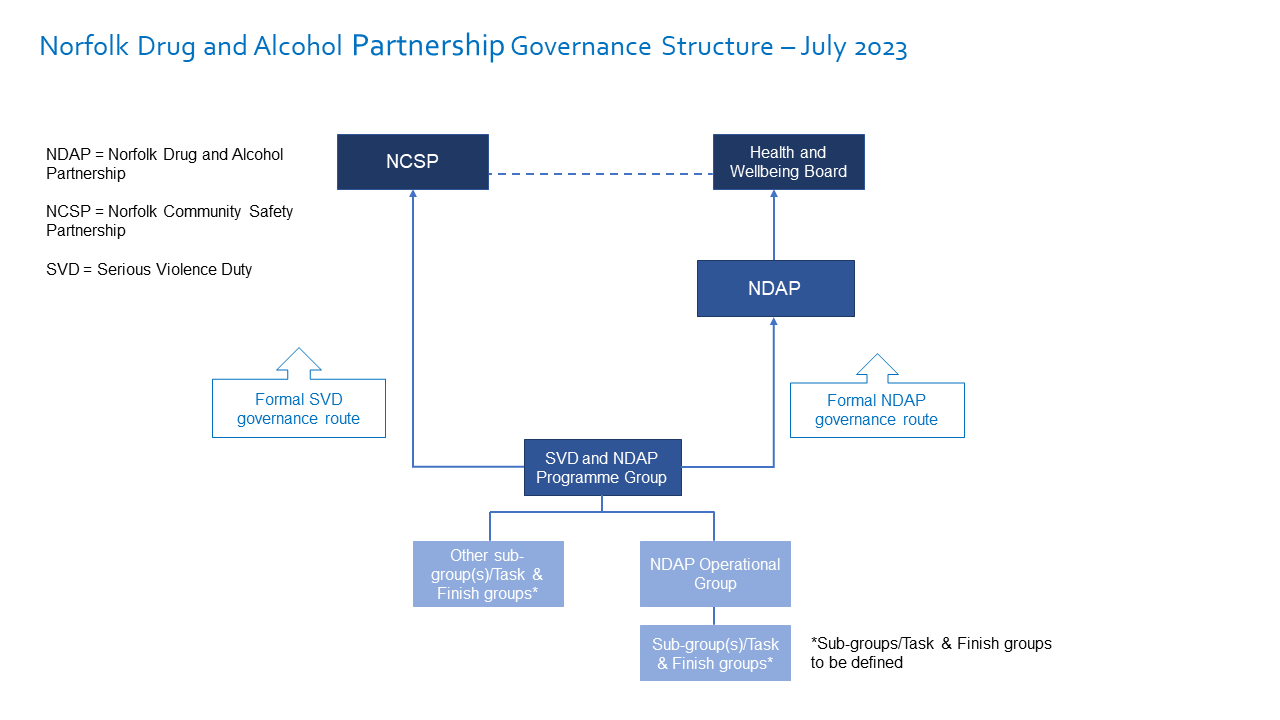
Norfolk drug and alcohol partnership governance structure as of July 2023
List of NDAP stakeholders:
- Norfolk County Council, including Public Health
- Norfolk Fire and Rescue Service
- Norfolk Constabulary
- Office of the Police and Crime Commissioner
- Norfolk Community Safety Partnership
- District and Borough Councils
- National Probation Service
- HM Prison Service
- Department of Work and Pensions
- Voluntary Norfolk
- NHS England
- Norfolk and Waveney Integrated Care Board
- Change, Grow, Live
- The Matthew Project
- Norfolk and Suffolk Foundation Trust
Dual Diagnosis
Our first priority is to try and tackle the issue of Dual Diagnosis. Dual Diagnosis means that someone has both a mental health problem and a drug/alcohol problem.
We are working with our NHS colleagues, the ICB or Integrated Care Board, to develop a clear pathway between both mental health and drug and alcohol services. This means that people will be able to get treatment for both of their problems at the same time. It should also mean that the care they receive is joined up and that information is shared between the services. This should mean that they receive better care and hopefully recover quicker.
This year we aim to:
- Establish a multiagency group to take this forward
- Work with people who have lived experience of dual diagnosis to capture their views
- Collect better data around dual diagnosis in Norfolk
- Find out what training is already available around this subject and how we can make sure it is available to those that need it
- Agree a direct pathway between our drug and alcohol service (CGL) and our mental health service (NSFT)
Prison to Community Continuity of Care
People who have been detained in prison are able to access drug and alcohol treatment just as they would in the community.
To ensure that their treatment continues seamlessly when they leave prison, we need to make sure that they can easily access the services and resources they need when they leave prison.
People are very vulnerable when they leave prison as they may not have stable accommodation, finances, employment or family to go back to. This means that they often start using drugs and alcohol again. This often leads them back into a life of crime and further time in prison—a revolving door from which it is difficult to escape.
NDAP is focusing on this area to improve outcomes for people in prison and to reduce demand and costs to our services through repeat offending.
This year we aim to:
- Increase the number of people that are receiving treatment and taking part in recovery focused activities in prison
- Increase the number of people who leave prison and transfer into community drug and alcohol services. We also want to make sure that these people stay in treatment and successfully complete their treatment journey.
- Improve joint working between prison and community teams
- Develop pathways for people leaving prison who have a dual diagnosis of drug and alcohol misuse and mental health need.
Training and Workforce Development
Making sure our workforce is properly trained is vitally important if we want to improve outcomes for people that use our services.
In Norfolk, we have identified that there is a need for more training and development opportunities for individuals and organisations in order to improve the quality of our service and to help recruit and retain staff. This is particularly important since we have had higher turnover of staff as a result of the Covid pandemic.
Our service users have told us that the stigma attached to substance misuse can often stop them from seeking help. We are working with our providers and the wider community to break down these barriers.
The new Drug Strategy is clear that we need to invest in our workforce to build knowledge and skills.
This year we aim to:
- Establish a specialist working group that will lead on this work
- Carry out a training audit which will help us identify any gaps in skills and knowledge
- Identify existing training opportunities that can be shared across the workforce
- Develop new training opportunities to fill any gap
- Explore the possibility of a dedicated training coordinator for Norfolk
Countywide rollout of Project ADDER
The Project ADDER (Addiction, Diversion, Disruption, Enforcement and Recovery) pilot programme ran for three years in the Greater Norwich area and finished in March 2023. After a successful three-year pilot, a decision was made to fund the programme for a further two years from our national funding allocation. The programme will now run until March 2025 and will roll out across the county.
Any drug or alcohol-related death is a tragedy and impacts the lives of individuals, families and communities. The national drugs strategy, From Harm to Hope makes a government-wide commitment to preventing 1,000 drug-related deaths by 2024 to 2025.
Most drug deaths are cause by opioids such as heroin. Across England, drug deaths have been rising which is mainly due to an aging cohort of heroin users who are now experiencing the effects of decades of prolonged use. As well as the impact on their physical and mental health, this also makes them susceptible to overdose.
Prolonged drinking over time can lead to a number of health conditions including liver disease, cancer and heart disease. Over half of alcohol-related deaths are because of health effects from drinking too much over time. Alcohol deaths can also occur as a direct consequence of drinking through alcohol poisoning or alcoholic liver disease.
This year we aim to:
- Establish a robust Local Drug Information System (LDIS) in order to share alerts around drugs in circulation, issues with strength, contaminated batches etc
- Establish a multiagency panel to review drug- and alcohol-related deaths
- Work on collecting Real Time Surveillance data
- Agree ways in which we can share data with partners about non-fatal overdoses
The Ready to Change website offers people the opportunity to make small changes to improve their health. Click here to get help to drink less:
Help to drink less - Norfolk County Council
Get help with drug and alcohol use:
Need help? - Norfolk County Council
Alcohol, drugs and mental health: click here to find out more:
Alcohol drugs and mental health - Norfolk County Council
Norfolk Insight - Norfolk's Joint Strategic Needs Assessment which provides data and analysis for neighbourhoods in Norfolk and Waveney. Click here to access reports, papers, profiles and needs assessments that inform Norfolk's JSNA.